Michael L. Sweeney,
1,2 Logan D. Vance,1 Stacy L. Sweeney,
1 Delina H. Bishop1,2
- OPTI Health Lake Norman, Mooresville, NC USA
- OPTI Health Research Institute dba OPTIVets, Mooresville, NC, USA
I. Executive Summary
This paper presents a comprehensive, evidence-based multi-modal treatment approach, known as The OPTIprotocol, designed to improve outcomes for Veterans and First Responders (participants) suffering from Post-Traumatic Stress Disorder (PTSD), Traumatic Brain Injury (TBI), and extreme environmental and pulmonary toxin exposure conditions such as burn pit exposure. Utilizing a combination of Hyperbaric Oxygen Therapy (HBOT), Intermittent Hypoxic-Hyperoxic Training (IHHT) aka Exercise with Oxygen Training (EWOT), photobiomodulation (red light therapy), neurofeedback, NAD+ IV infusions, oral supplementation, and health coaching, this approach has shown significant improvements in clinical outcomes. Key findings include reductions in PTSD symptoms, depression, and sleep disturbances, along with improved cognitive-emotional functioning, brain plasticity, and anger management. The results demonstrated in this paper advocate for the adoption of this multi-modal strategy in Veteran healthcare programs which aim to improve the quality of life for Veterans and First Responders facing these complex challenges.
II. Introduction
Veterans and First Responders often suffer from a combination of PTSD and TBIs due to the nature of their work. Exposures to extreme environmental toxins like burn pits, chemical contaminants, and smoke are also common in these communities. These conditions frequently lead to a variety of debilitating symptoms, including chronic pain, migraines, sleep disturbances, mood disorders, and cognitive impairments. Traditional treatment approaches, which often rely heavily on pharmacological interventions and psychotherapy, have had limited success in addressing the complex interplay of symptoms these Veterans and First Responders face.5
This paper introduces The OPTIprotocol, a multi-modal therapeutic model that integrates physical, cognitive, emotional, and neurophysiological treatments. The objective is to provide a more holistic solution to PTSD and TBI treatment, addressing not only the mental health component but also the neurological and physiological damage caused by combat trauma and environmental exposures.
III. The Need for a Multi-Modal Approach
Current Treatment Gaps
Despite advances in pharmacological treatments for PTSD and TBI, many Veterans and First Responders continue to suffer from residual or unmitigated symptoms that severely impact their daily lives. Common treatments, such as antidepressants and cognitive-behavioral therapy (CBT), may address symptoms like depression and anxiety, but they fail to tackle the underlying physical, chemical, and neurological damage from PTSD, TBIs and/or the systemic effects of environmental toxins.5
Veterans and First Responders also frequently experience sleep disturbances, chronic pain, migraines, and mood dysregulation, which are poorly addressed by standard treatments. The need for a comprehensive approach that tackles both the psychological, physiological, and physical dimensions of these conditions has never been more desperate.
Rationale for Integration
A multi-modal approach recognizes that PTSD and TBI affect multiple systems in the body and brain, necessitating therapies that work synergistically. By combining modalities such as HBOT, IHHT, and neurofeedback, which directly promote brain repair and neuroplasticity, with supportive treatments like NAD+ IV infusions, red light therapy, and targeted supplementation, this approach can provide more complete symptom relief. Professional health coaching further enhances outcomes by promoting incremental lifestyle changes that reinforce the healing benefits of the treatment modalities.
IV. Components of the Multi-Modal Treatment Approach
- Hyperbaric Oxygen Therapy (HBOT)
HBOT involves the administration of concentrated oxygen in a pressurized chamber, promoting neuroplasticity through angiogenesis, neurogenesis, and inflammation reduction.10,22 In this treatment, oxygen was delivered using a built-in breathing system (BIBS) at 93%+ oxygen concentration during 60-minute sessions at an average pressure of 1.8 ATA.22,23 Sessions were conducted daily and occasionally 2x daily with a minimum 4-hour break between sessions when participant schedules required flexibility. Critical to treating PTSD and TBI symptoms are the HBOT’s physiological mechanisms, including its angiogenic, antimicrobial, and immunomodulatory properties.17,23 This study can reinforce the scientific basis for using HBOT to enhance tissue oxygenation, promote neuroplasticity, and reduce inflammation, which are critical for treating PTSD and TBI symptoms.10,22 This modality has been shown in numerous studies to improve cognitive function, reduce PTSD symptoms, and aid in the healing of brain tissues affected by TBI.9,10,13,16,22
2. Intermittent Hypoxic-Hyperoxic Training (IHHT) and/or Exercise with Oxygen Therapy (EWOT)
IHHT involves alternating between breathing oxygen-rich and oxygen-depleted (high altitude simulated) air while EWOT alternates between normal and high oxygen concentrations while exercising. To date, the medical, research, and equipment manufacturer communities often oscillate between both acronyms. For this study, we utilized a combination of the two approaches, where high oxygen concentrations were used in conjunction with low concentrations while exercising for 15 minutes on a stationary bike. By activating the body’s hypoxic induction factors (HIFs) through intermittent hypoxia, cell signaling upregulates the production of red and white blood cells as well as progenitor stem cell release.2 The hyperoxic portion of the exercise regimen, similar to hyperbaric oxygen, stimulates mitochondrial function, ATP production, and cellular repair. This technique enhances energy metabolism, improves oxygen utilization, and promotes resilience to stress—key factors in brain injury recovery.1,21
Additionally, the high intensity interval training (HIIT) aspects of IHHT/EWOT increase the production and release of brain derived neurotrophic factor (BDNF).1 BDNF is crucial for the survival and development of neurons.1 It acts as a neurotransmitter modulator and contributes to neuronal plasticity, a key process for learning and memory. BDNF is widely present in the central nervous system, gut, and other tissues.3
3. Photobiomodulation (Red Light Therapy)
Red light therapy stimulates cellular repair and reduces inflammation through the application of specific wavelengths of light through the skin targeting the circulatory system, muscles, organs, and brain.26 Research shows that photobiomodulation can improve cognitive functioning, support brain recovery in TBI patients, and alleviate mood disorders by enhancing mitochondrial activity in neurons.11
4. Neurofeedback
QEEG guided neurofeedback trains the brain to self-regulate by using real-time feedback on brainwave activity.12 Participants with PTSD and TBIs often exhibit significantly dysregulated brainwave patterns, which contribute to anxiety, mood disorders, and cognitive impairment.8,12 Neurofeedback training helps reorganize these brainwave patterns, leading to better emotional regulation, improved sleep, and enhanced cognitive clarity.8,12
Alpha/Theta Neurofeedback, or lower frequency neurofeedback, uses oscillations between an alpha wave and theta wave to process hard emotions.12 It also helps with peak performance, creativity, and overall relaxation.8 Participants in the OPTIprotocol experience 30 Alpha/Theta sessions, following higher frequency training. At the end of the Protocol, higher frequency training is resumed.
5. NAD+ IV Infusions plus Glutathione
Nicotinamide adenine dinucleotide (NAD) plays a crucial role in cellular repair and mitochondrial function. Throughout the study, eight NAD+ intravenous infusions followed by IV glutathione, the liver’s primary and most powerful antioxidant, were administered to participants to enhance cellular recovery, reduce oxidative stress, and support overall brain function and repair. This therapy has been particularly effective in mitigating the cognitive decline, mood lability, and fatigue by enhancing mitochondrial function and energy metabolism in individuals with PTSD and TBI.7,19
6. Oral Supplementation
Participants received a 90-day course of oral supplements that included prebiotics, probiotics, and nootropics. These supplements were designed to enhance gut health, reduce systemic inflammation, improve cognitive performance, mood, and motivation by supporting the gut-brain axis, a critical pathway in mental health. All supplements are approved by the Banned Substance Control Group (BSCG), received the highest rated third-party certification, and were tested for banned substances. Focus on the gut-brain axis can reduce inflammation and support mental health improvement such as demonstrated reductions in anxiety and depression scores.4,15,18,20
7. Health Coaching and Lifestyle Interventions
Health coaching sessions, performed by National Board Certified Health Coaches, focused on optimizing sleep, diet, and thought patterns. These interventions reinforced the physiological treatments by addressing underlying lifestyle factors that contribute to chronic symptoms in PTSD and TBI. Burback et al. discuss the role of chronic stress and allostatic load in PTSD, which reinforces the focus on health coaching to promote lifestyle changes that mitigate chronic stress.5 Coaching provides participants with tools for long-term lifestyle changes and promotes sustained improvements that have been shown to be sustainable.14 Participants received their own coaching handbook, OPTIprotocol Sleep Manual, and shopping lists for brain healthy foods.
V. Assessment Tools
PCL-5: The Post-Traumatic Stress Disorder Checklist for DSM-5 is a 20-item self report measure that assesses the presence and severity of PTSD symptoms.25 Items on the PCL-5 correspond with diagnostic and statistical manual (DSM-5) criteria for PTSD.
PQH-9: The PHQ-9 is a multipurpose instrument for objectively determining severity of initial depressive symptoms, while also allowing for the monitoring of symptom changes and effects of treatment over time. It is not, however, a diagnostic tool. Results from the PHQ-9 must be used in conjunction with clinical judgment and other data as required to reach the appropriate conclusion.
QEEG: Quantitative electroencephalography (qEEG) is an advanced method of EEG analysis that records digital EEG signals, which are then processed and analyzed with sophisticated mathematical algorithms. qEEG enables new ways to extract features from EEG signals, including analysis of specific frequency bands, signal complexity, connectivity, and network functions. Clinically, qEEG is widely applied in assessing neuropsychiatric disorders, epilepsy, stroke, dementia, traumatic brain injury, mental health conditions, and more.
CEC: A Cognitive Emotional Checklist is an assessment tool used to evaluate an individual’s cognitive and emotional functioning. It typically measures factors such as emotional regulation, thought patterns, cognitive flexibility, and stress responses. By identifying specific areas of cognitive or emotional difficulties, the checklist helps clinicians understand a person’s mental state and tailor interventions to improve emotional well-being and cognitive resilience. It is often used in therapeutic settings to track changes in cognitive-emotional health over time.
VI. Case Study Results: Impact on Participant Health
A 12-week study involving seven Veterans with varying degrees of PTSD, TBI, and extreme environmental exposure demonstrated the significant positive impact and effectiveness of this multi-modal approach:
- PCL-5 (PTSD Assessment): Scores decreased significantly across all participants, with pre-OPTIprotocol scores ranging from 18 to 76, mid-treatment scores ranging from 2 to 44, and post-treatment scores ranging from 3 to 15. These reductions indicate a shift from severe PTSD symptoms to below-threshold levels, with all post-protocol scores under 35, representing less than a 15% probability of PTSD. (Lower score consistent with lower chance of PTSD symptoms)
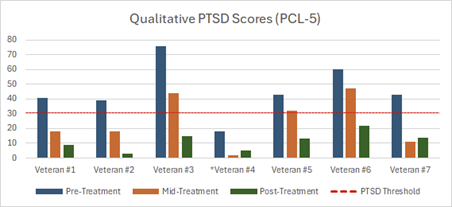
* Veteran was diagnosed with multiple TBIs and did not meet the threshold for PTSD
- PHQ-9 (Depression Assessment): Pre-treatment scores ranged from 7 to 23, indicating moderate to severe depression. By mid-protocol, scores had decreased to a range of 0 to 15, and post-protocol scores further reduced to 0 to 7, reflecting a transition from moderate to minimal depression levels across all participants. (Lower score consistent with lower chance of depression symptoms)
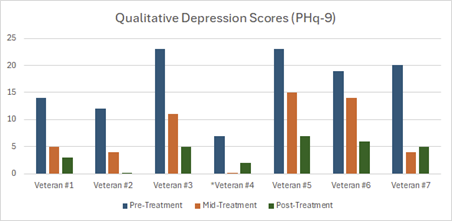
* Veteran was diagnosed with multiple TBIs and did not meet the threshold for PTSD
- PSQI (Sleep Quality Assessment): Pre-protocol PSQI scores varied, with mid-protocol averages around 6-8 and post-protocol averages between 3 and 7. post-treatment, most participants achieved scores below 5, indicating significant improvements in sleep quality.
- qEEG Brain Mapping (Neuroplasticity and Normalization): Neurofeedback data revealed outstanding plasticity and normalization improvements. Mid-protocol plasticity scores ranged from 29% to 42%, with post-protocol increases up to 50%. Similarly, normalization scores ranged from 35% to 52% by mid-protocol, with post-treatment normalization maintained between 39% and 51%. These results highlight significant brain plasticity and normalization improvements associated with the treatment.
- Cognitive Emotional Checklist (CEC): Participants reported improvements in cognitive and emotional issues, with pre- to post-protocol changes ranging from 17% to 86%. Improvements were consistently observed in areas such as memory, emotional regulation, thought patterns, and focus, with most participants reporting over 50% improvement in several domains.
- Veteran #5 reported complete resolution of suicidal ideation and significant improvement in pulmonary function.
- Veteran #7 reported vastly better emotional regulation, decreased anger, and complete resolution of suicidal ideation. Additionally, Veteran #7 reconnected with estranged family members throughout the Protocol.
- Veterans #1 and #4 reported resolution of migraine symptoms.
- Veteran #4 also reported no longer requiring pain medications that had once been a twice daily occurrence.All participants reported sleeping at least 7 hours at night
- Veteran #6 reported a constant pain score of 7-8/10 pre-Protocol and 4-5/10 intermittent pain post-Protocol
- Veteran #1 showed the following data, based on his wearable device:
- Increase in average deep sleep from 7 to 42 minutes
- 13.5% decrease in resting heart rate
- 14.2% improvement in cardio fitness level
- Veteran #2 reported sleep improved from 3-4 hours to 7-8 hours nightly
- Veteran #2 had an increase in skeletal muscle mass by 3 pounds and decreased body fat by 2.5%.
Overall, the aggregated data support the efficacy of the multi-modal OPTIprotocol, demonstrating significant reductions in PTSD and depression symptoms, improved sleep quality, enhanced brain plasticity and normalization, and improved cognitive-emotional function. These findings underscore the comprehensive benefits of integrating therapies such as HBOT, IHHT/EWOT, photobiomodulation, neurofeedback, NAD+ infusions, and oral supplementation with health coaching for Veterans with PTSD, TBI, and related comorbidities.
VII. Scientific Rationale and Supporting Evidence
Neuroplasticity and Cognitive Recovery
HBOT, IHHT/EWOT, and neurofeedback have all been shown to promote neuroplasticity, or the brain’s ability to adapt and repair itself.1,13,16,21 These therapies enhance cognitive recovery by stimulating the growth of new neurons, increasing oxygen supply to the brain, and retraining dysregulated brainwave patterns.1,13,21 The research by Doenyas-Barak et al. highlights significant improvements in brain activity and microstructural integrity in regions such as the hippocampus and prefrontal cortex.9 HBOT upregulates growth factors like VEGF and increases nitric oxide levels, leading to improved angiogenesis and cellular repair.17,23 Tal et al. provide clinical evidence demonstrating the capacity of HBOT to increase cerebral blood flow and regenerate nerve fibers in TBI patients, emphasizing its role in enhancing brain recovery and reducing long-term cognitive impairment.23 Hatch et al. discusses significant SPECT imaging findings, showing normalization of brain blood flow patterns and improved texture, which underscores the neurophysiological benefits of HBOT.13 Proper supplementation aids neuroplasticity and improves cognitive recovery by directly affecting regions of the brain associated with stress and memory.6,7
Inflammation and Mitochondrial Support
Photobiomodulation and NAD+ infusions work synergistically to reduce inflammation and support mitochondrial health, essential for brain recovery after injury.11 These therapies help restore cellular function and reduce the oxidative damage that contributes to PTSD and TBI symptoms.7 By improving mitochondrial function, NAD+ can help alleviate the neurodegenerative and inflammatory processes associated with TBI and PTSD.19
HBOT/IHHT and Red Light
Oxygen and red light work together within the mitochondria to enhance ATP production, which is where most cellular energy is generated.26 Oxygen serves as the final electron acceptor in the electron transport chain, a critical step in energy synthesis. Red light, on the other hand, stimulates key mitochondrial proteins, such as cytochrome c oxidase, which allows for more efficient electron transfer, ultimately resulting in increased ATP production.26 In essence, oxygen provides the necessary component for the final stage of ATP synthesis, while red light optimizes the process by activating the mitochondrial machinery involved in electron transport.26
Gut-Brain Axis
Emerging research has highlighted the importance of gut microbiome health in mental well-being. Probiotic and prebiotic supplementation supports the gut-brain axis, improving mood, motivation, cognitive function, and inflammation management by regulating the microbiome.2 Reducing stress responses can be done by using dietary interventions to manage stress and promote cognitive and emotional stability.24 Pivac et al. discuss the dysregulated hypothalamic-pituitary-adrenal (HPA) axis, chronic low-grade inflammation, and oxidative stress in PTSD patients and that integrating anti-inflammatory strategies, such as targeted supplementation and health coaching, will address systemic inflammation and improve overall health outcomes.18 Additionally, Savignac et al. provides evidence on the impact of prebiotics to reduce inflammation and modulate anxiety behaviors.20
VIII. Comparison with Conventional Treatments
Limitations of Pharmacological Approaches
Pharmacological treatments, while effective for some symptom management, often come with side effects and fail to address the root causes of PTSD and TBI.5 Antidepressants and sedatives may temporarily reduce anxiety or depression to some degree, but they do not promote brain healing or improve cognitive function.5
Cost-Benefit Analysis
The OPTIprotocol multi-modal approach offers a long-term cost-saving benefit by reducing the need for chronic medication, hospital visits, and disability support. Participants experience improved quality of life leading to fewer healthcare resources required over time. A comprehensive $18,000 program for treating PTSD and TBI offers a more cost effective solution compared to the traditional methods employed today. Veterans supported through conventional methodologies often face repeated hospitalizations, long-term medication use, and ongoing therapies, which can accumulate costs rapidly as time goes on. Indirect costs, such as lost productivity, reliance on benefits, and strained support systems, add to the financial burden. Investing in the 12-week Protocol eliminates much of the need for continuous support leading to faster, more sustainable outcomes with significant monetary savings.
IX. Policy Implications and Recommendations
Advocating for Change
The demonstrated success of this multi-modal approach suggests it should be integrated into Veteran healthcare programs. Healthcare providers should consider adopting this model, which has proven to improve physical, emotional, and cognitive outcomes for Veterans and First Responders suffering from complex conditions.
Collaboration with Veteran Affairs and Other Institutions
Partnerships between military and Veteran healthcare institutions, private healthcare providers, and research institutions can foster the implementation of this approach on a broader scale. Increased funding for further research and treatment expansion is necessary to make this approach accessible to all participants.
X. Conclusion
The OPTIprotocol, a multi-modal therapeutic approach, offers significant improvements in PTSD, TBI, and related conditions for participants, targeting both physical and cognitive symptoms. The OPTIprotocol integration into healthcare programs can lead to improved outcomes, reduced healthcare costs, and enhanced quality of life for participants. We urge healthcare providers, researchers, and policymakers to adopt and support this innovative model.
XI. References
- Bayer U, Likar R, Pinter G, et al. Intermittent hypoxic-hyperoxic training on cognitive performance in geriatric patients. Alzheimers Dement (N Y). 2017;3(1):114-122. Published 2017 Feb 8. doi:10.1016/j.trci.2017.01.002
- Behrendt T, Bielitzki R, Behrens M, et al. Effects of intermittent hypoxia–hyperoxia on performance- and health-related outcomes in humans: a systematic review. Sports Med Open. 2022;8:70 doi:10.1186/s40798-022-00450-x.
- Bekinschtein P, Cammarota M, Medina JH, BDNF and Memory Processing, Neuropharmacology, Volume 76, Part C, 2014, Pages 677-683, ISSN 0028-3908, https://doi.org/10.1016/j.neuropharm.2013.04.0 24.
- Brenner LA, Forster JE, Stearns-Yoder KA, et al. Evaluation of an immunomodulatory probiotic intervention for veterans with co-occurring mild traumatic brain injury and posttraumatic stress disorder: A pilot study. Front Neurol. 2020;11:1015. doi:10.3389/fneur.2020.01015.
- Burback L, Brémault-Phillips S, Nijdam MJ, McFarlane A, Vermetten E. Treatment of posttraumatic stress disorder: a state-of-the-art review. Curr Neuropharmacol. 2024;22(4):557-635. doi:10.2174/1570159X21666230428091433.
- Ceremuga TE, Martinson S, Washington J, et al. Effects of L-theanine on posttraumatic stress disorder induced changes in rat brain gene expression. ScientificWorldJournal. 2014;2014:419032. doi:10.1155/2014/419032
- Cuenoud B, Ipek Ö, Shevlyakova M, et al. Brain NAD is associated with ATP energy production and membrane phospholipid turnover in humans. Front Aging Neurosci. 2020;12:609517. doi:10.3389/fnagi.2020.609517.
- Dahl MG. Neurofeedback with PTSD and traumatic brain injury (TBI). In: Kirk HW, ed. Restoring the Brain: Neurofeedback as an Integrative Approach to Health. Routledge; 2020:256-284. doi:10.4324/9780429275760-13.
- Doenyas-Barak K, Catalogna M, Kutz I, et al. Hyperbaric oxygen therapy improves symptoms, brain’s microstructure and functionality in veterans with treatment resistant post-traumatic stress disorder: A prospective, randomized, controlled trial. PLoS One. 2022;17(2). Published 2022 Feb 22. doi: 10.1371/journal.pone.0264161.
- Hadanny A, Abbott S, Suzin G, Bechor Y, Efrati S. Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post-traumatic brain injury patients: retrospective analysis. BMJ Open. 2018 Sep 28;8(9). doi:10.1136/bmjopen-2018-023387. PMID: 30269074; PMCID: PMC6169752.
- Hamblin MR. Photobiomodulation in the brain: low-level laser (light) therapy in neurology and neuroscience. In: Hamblin MR, ed. Photobiomodulation in the Brain: Low-Level Laser (Light) Therapy in Neurology and Neuroscience. Academic Press; 2019:1-630. doi:10.1016/C2017-0-02758-1.
- Harch PG, Andrews SR, Fogarty EF, Lucarini J, Van Meter KW. Case control study: hyperbaric oxygen treatment of mild traumatic brain injury persistent post-concussion syndrome and post-traumatic stress disorder. Med Gas Res. 2017;7(3):156-174. Published 2017 Oct 17. doi:10.4103/2045-9912.215745.
- Kivelä K, Elo S, Kyngäs H, Kääriäinen M. The effects of health coaching on adult patients with chronic diseases: A systematic review, Patient Education and Counseling, Volume 97, Issue 2, 2014, Pages 147-157, ISSN 0738-3991, https://doi.org/10.1016/j.pec.2014.07.026.
- Messaoudi M, Violle N, Bisson JF, Desor D, Javelot H, Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes. 2011;2(4):256-261.
doi:10.4161/gmic.2.4.16108 - Mozayeni BR, Duncan W, Zant E, Love TL, Beckman RL, Stoller KP. The National Brain Injury, Rescue and Rehabilitation Study – a multicenter observational study of hyperbaric oxygen for mild traumatic brain injury with post-concussive symptoms. Med Gas Res. 2019;9(1):1-12.
doi:10.4103/2045-9912.254636. - Ortega MA, Fraile-Martinez O, García-Montero C, et al. A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina (Kaunas). 2021;57(9):864. Published 2021 Aug 24. doi:10.3390/medicina57090864
- Pivac N, Vuic B, Sagud M, et al. PTSD, immune system, and inflammation. Adv Exp Med Biol. 2023;1411:225-262. doi:10.1007/978-981-19-7376-5_11. PMID: 36949313.
- Pivac N, Vuic B, Sagud M, et al. PTSD, immune system, and inflammation. Adv Exp Med Biol. 2023;1411:225-262. doi:10.1007/978-981-19-7376-5_11. PMID: 36949313.
- Radenkovic D, Reason, Verdin E. Clinical Evidence for Targeting NAD Therapeutically. Pharmaceuticals (Basel). 2020;13(9):247. Published 2020 Sep 15. doi:10.3390/ph13090247
- Savignac HM, Couch Y, Stratford M, et al. Prebiotic administration normalizes lipopolysaccharide (LPS)-induced anxiety and cortical 5-HT2A receptor and IL1-β levels in male mice. Brain Behav Immun. 2016;52:120-131. doi:10.1016/j.bbi.2015.10.007
- Serebrovska TV, Serebrovska ZO, Egorov E. Fitness and therapeutic potential of intermittent hypoxia training: a matter of dose. Fiziol Zh (1994). 2016;62(3):78-91. doi:10.15407/fz62.03.078. PMID: 29569889.
- Sonners J. Oxygen Under Pressure. Independently published; 2020 Jan 14. ISBN: 978-1661251352.
- Tal S, Hadanny A, Sasson E, Suzin G, Efrati S. Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients. Front Hum Neurosci. 2017 Oct 19;11:508. doi: 10.3389/fnhum.2017.00508. PMID: 29097988; PMCID: PMC5654341.
- Unno K, Yamada H, Iguchi K, et al. Anti-stress Effect of Green Tea with Lowered Caffeine on Humans: A Pilot Study. Biol Pharm Bull. 2017;40(6):902-909.
doi:10.1248/bpb.b17-00141 - Weathers FW, Lee DJ, Thompson-Hollands J, Sloan DM, Marx BP. Concordance in PTSD symptom change between DSM-5 versions of the Clinician-Administered PTSD Scale (CAPS-5) and PTSD Checklist (PCL-5). Psychol Assess. 2022;34(6):604-609. doi:10.1037/pas0001130.
- Whitten A. The Ultimate Guide To Red Light Therapy. 2018, Archangel Ink.
ISBN-13: 978-1-7217-6282-8


